|
PhysiologyMaps Home > Cardiovascular main > Cardiac myocytes
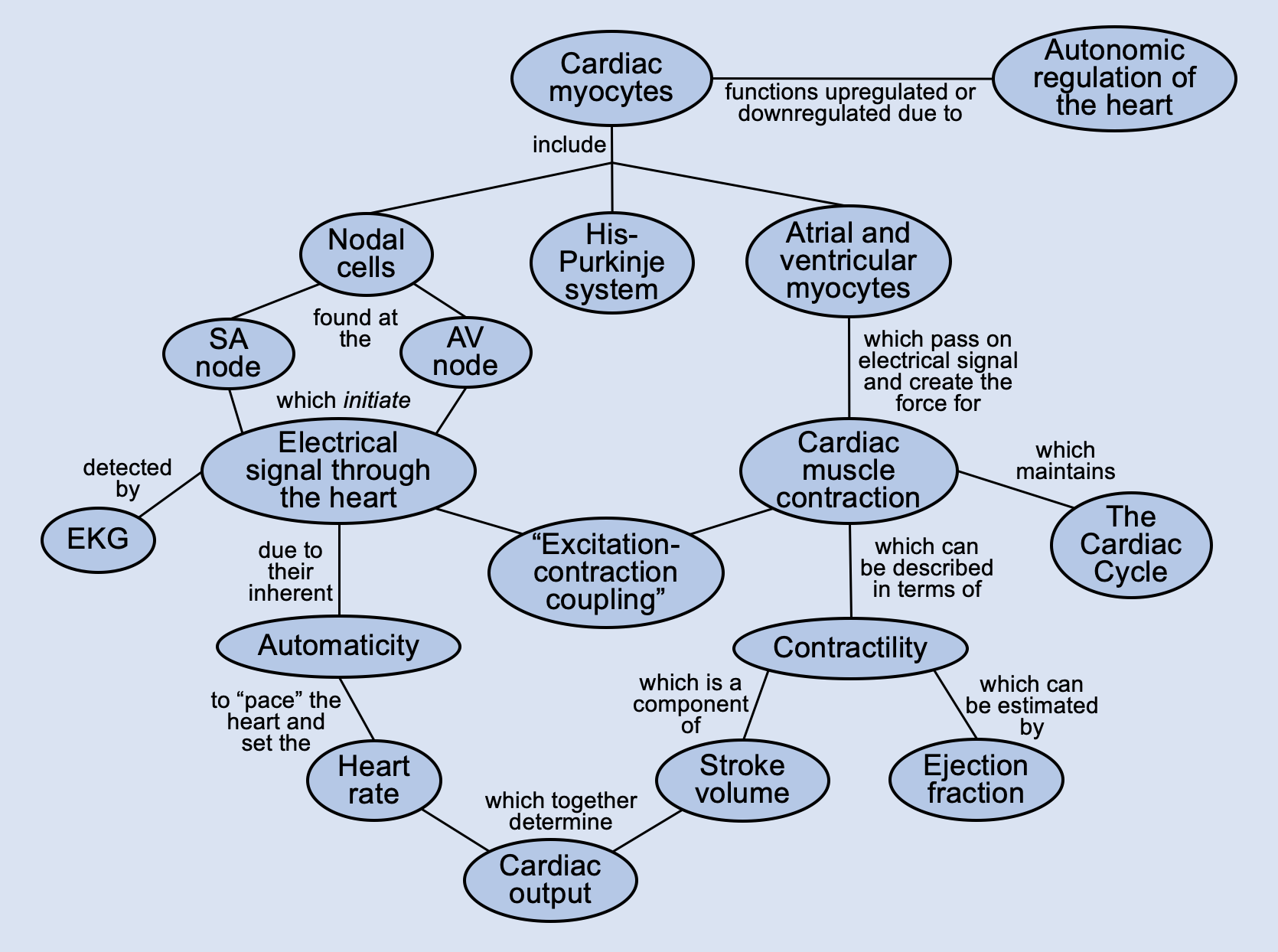
Automaticity of Cardiac Cells
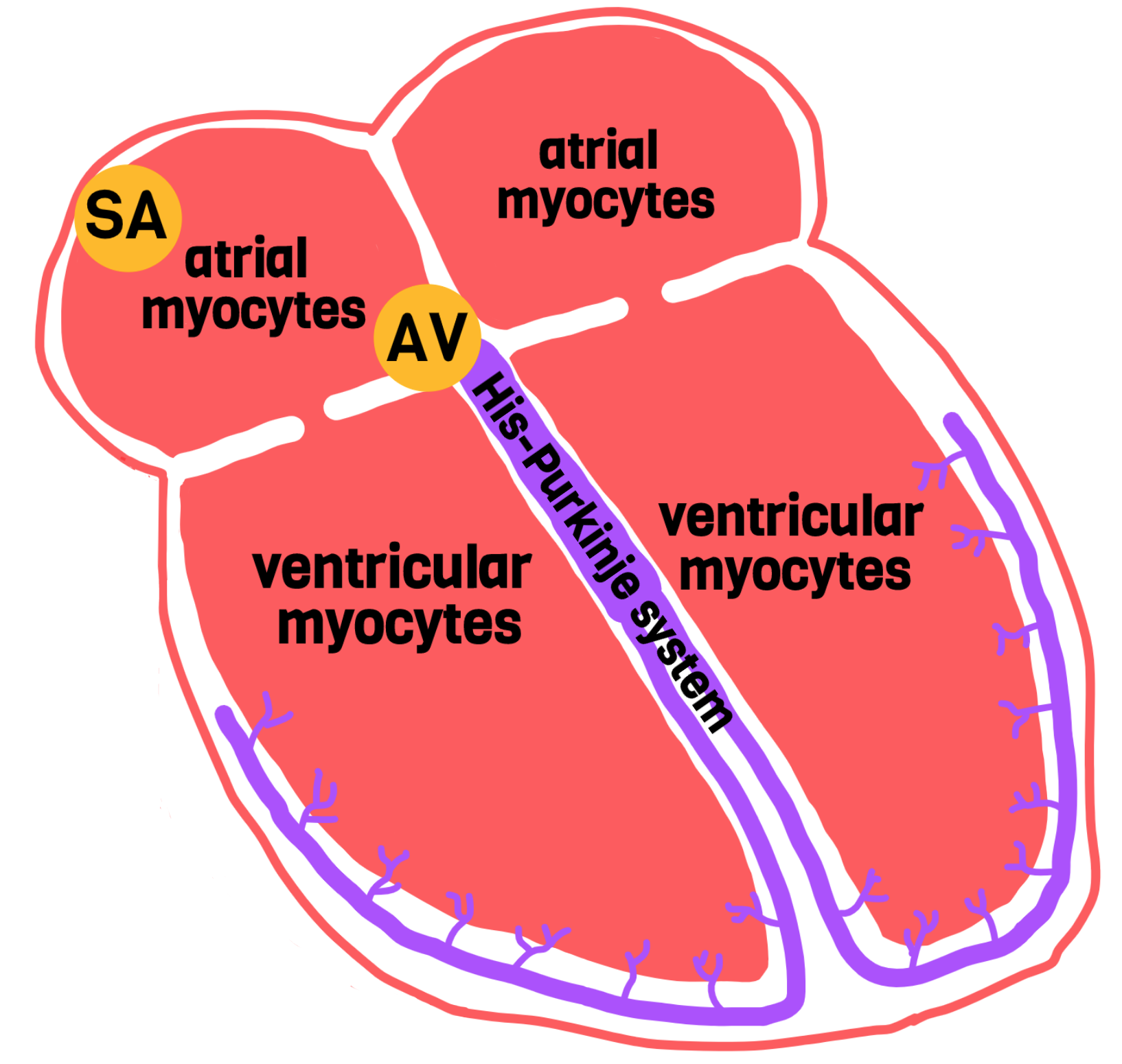
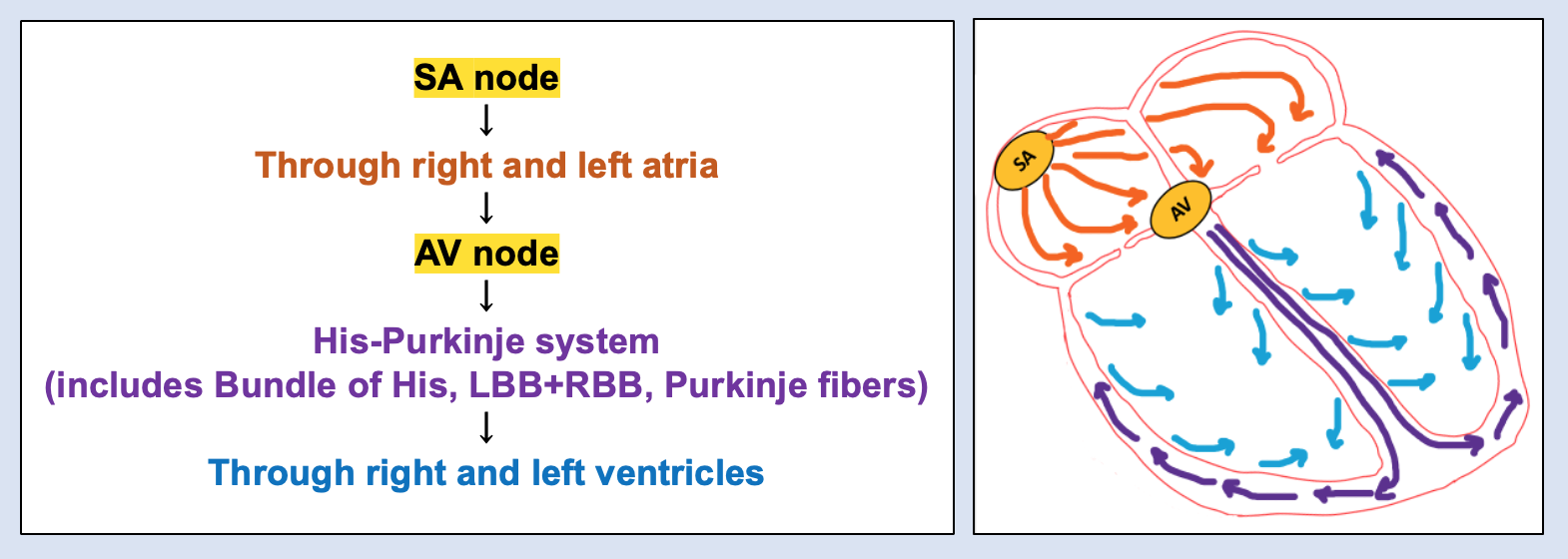
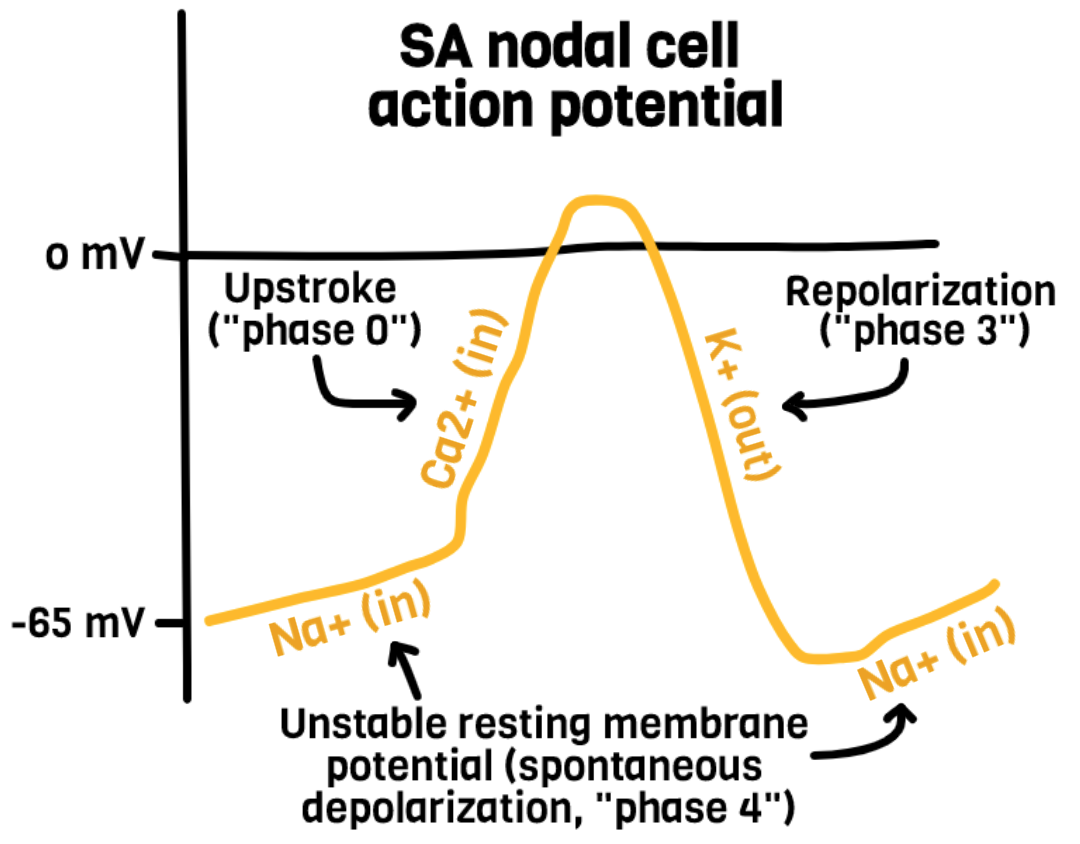
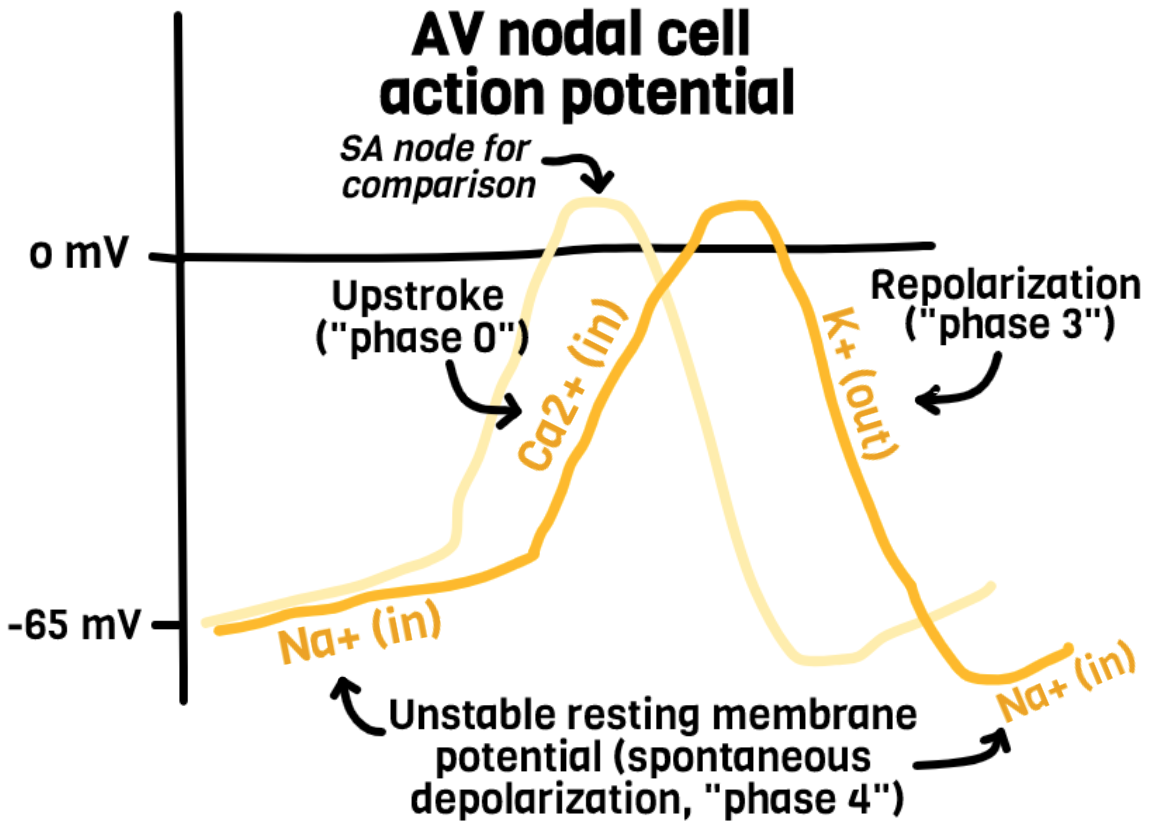
"Automaticity" refers to the ability of cardiac cells to spontaneously generate their own action potentials. In other words, they do not have to wait for a nearby cell to send it a signal in order to depolarize--they can depolarize on their own. SA nodal cells, AV nodal cells, and cells of the His-Purkinje system can all generate their own action potentials. However, they all have different firing rates.
The SA node has the fastest rate of spontaneous depolarization. This means that the SA node reaches its firing threshold more quickly than the AV node or His-Purkinje cells. So, under normal circumstances, the SA node will go off before the AV node ever reaches its firing threshold, and this will start the wave of depolarization throughout the heart. Therefore, the AV node doesn't need to use its automaticity function under normal circumstances: it will always just receive the signal traveling from the SA node first. This is why the SA node is considered the main pacemaker of the heart--it sets our resting heart rate by firing about once per second. Our normal resting heart rate is the typical firing rate of the SA node (60-90 beats per minute).
However, there are times when the SA node doesn't fire, or when the SA node's signal never reaches the AV node (eg, certain arrhythmias). In these situations, the AV node is not receiving any signal to depolarize from the SA node/atria. Thus, the AV node will just sit there, waiting to receive a signal; as the seconds tick on, the AV node's unstable resting membrane potential will finally reach its firing threshold and the AV node will depolarize on its own. This is essentially a back-up system for our heart: if something goes wrong with the SA node or the conduction in the first half of a heart beat gets messed up, the AV node has an escape route and can take over on its own. This way, our ventricles can still contract and keep our blood moving. This is why the AV node is considered the back-up pacemaker of the heart. However, whenever someone's AV node has to take over, they will likely present with bradycardia, since the automatic firing rate of the AV node is 40-60 beats per minute.
|